Complex psychological evaluation and correction methods of disorders in the emotional and personal sphere in children with post-COVID syndrome, considering structural and functional features of the brain
Troitskaya L.A.1, Plotnikova I.A. 2, Semenova N.D.1, Erokhina V.A.1, Plotnikova D.F.3, Avakyan G.G.1
1Pirogov Russian National Research Medical University, 1 Ostrovityanova st., 117997, Moscow, Russia.
2Ural State Medical University, 3 Repina st., 620014, Yekaterinburg, Sverdlovsk Oblast, Russia.
3Limited Liability Partnership “Tich’ I Spich Advance”, 28 Khadzhimukan st., 050059, Almaty, Kazakhstan.
*Corresponding author
*Inga A. Plotnikova, MD, PhD, Department of Pediatric Diseases, Ural State Medical University. inga63@bk.ru ORCID ID: 0000-0002-6909-1487.
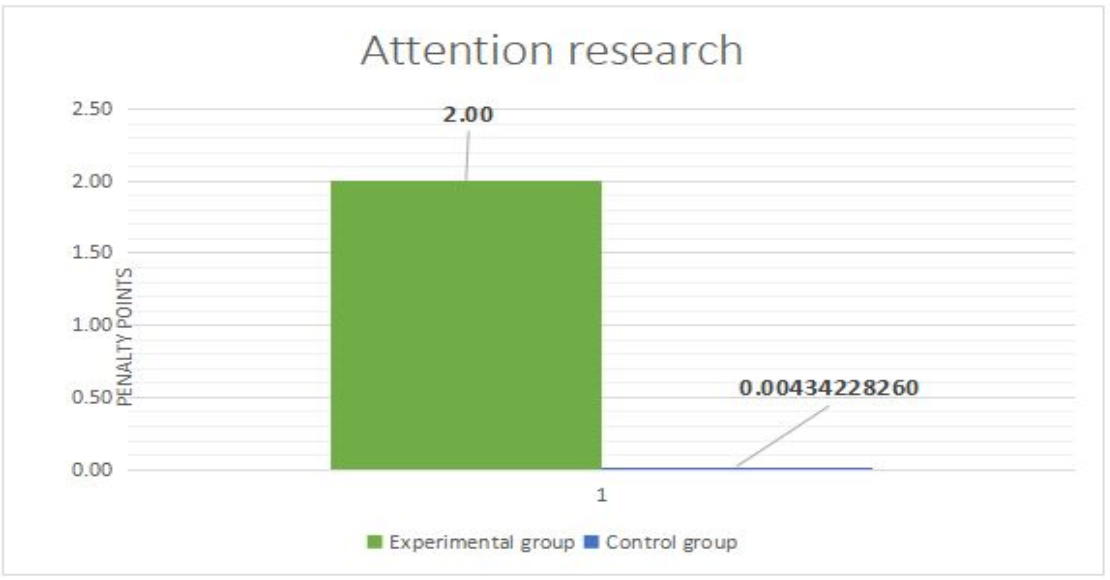
Figure 1: Neurodynamic component of mental activity.
- Mnestic functions in children of the main group.
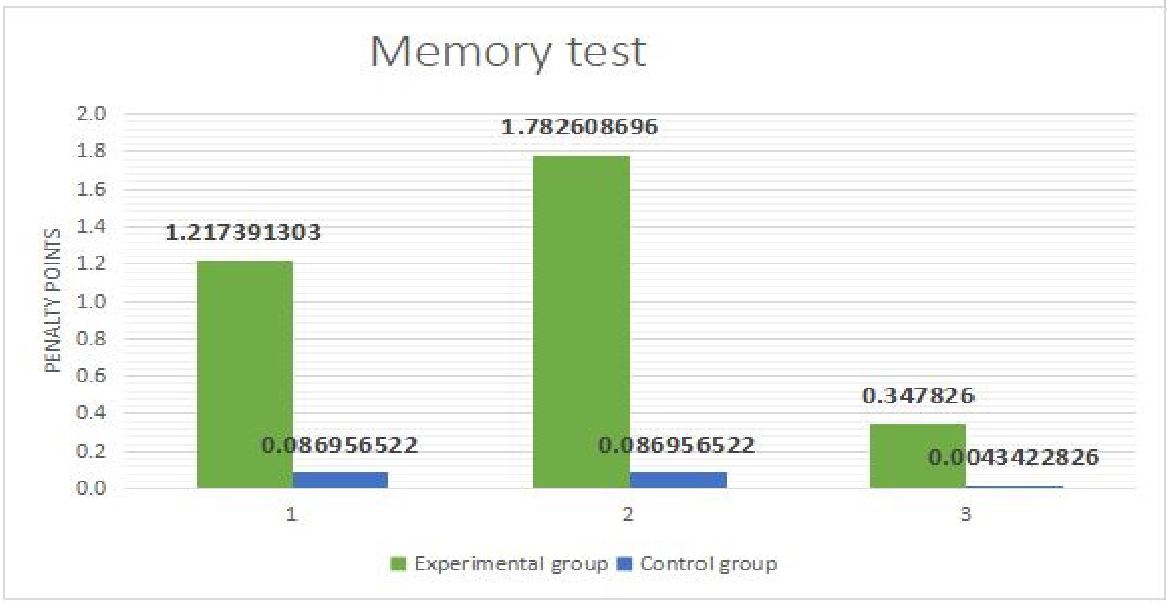
Significant statistical differences were revealed in the control group in the auditory-verbal direct memory test (1) (p=0.002) (Fig. 2). The nature of errors in memorizing 10 words included an increase in the latency period, verbal paraphasias ("'friend' instead of 'brother', 'pie' in place of 'cake'); verbal perseverations; lack of regulation and control.
When performing the test “Memorization of two phrases” (semantic memorization), the influence of heterogeneous interference, volume reduction and order disruption of representation, changes in the grammatical structure of speech (by gender, number, case) were observed.
The lesion was in mediobasal frontotemporal parts of the brain with the formation of the leading temporal neuropsychological syndrome (T2).
Figure 2: Mnestic functions of different modalities - auditory verbal and visual memorization: direct memorization (1), memorization of two phrases (2) and visual memorization (3) of the main and control groups.
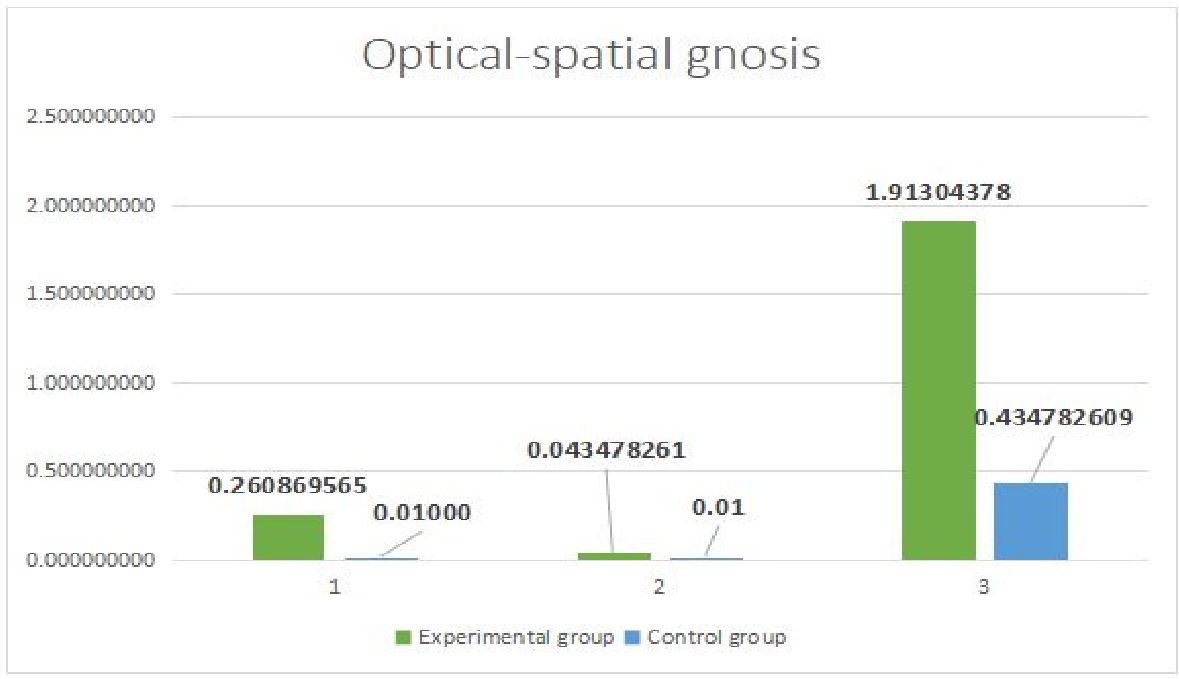
Optical-spatial gnosis
The success of performance in performing opto-spatial gnosis tests was significantly different in the main and control groups. In Figure 3: 1 - recognition of crossed-out images (p=0.265), H=2.659<Hcr; 2 - recognition of superimposed images (p=0.434); 3 - recognition of underdrawn images (p<0.001), H=18.377 >Hcr.
The test for identifying unfinished images, which requires the realization of a complete image, allows us to assess the formation of a holistic strategy of information processing. In result, simultaneous agnosia was revealed. Affected areas were the temporo-parietal-occipital regions of the brain.
Figure 3: The study of optical-spatial gnosis
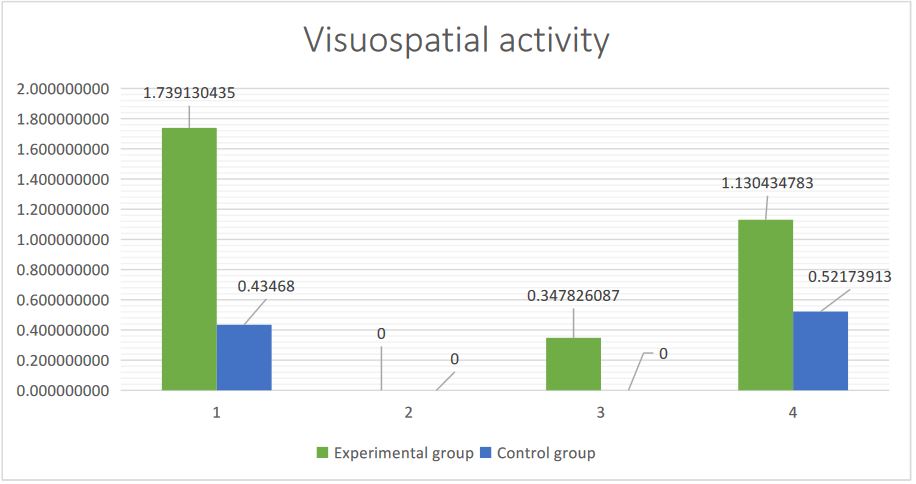
Graphic praxis.
A battery of neuropsychological methods was used to study visual-spatial gnosis and praxis, including copying (houses, figures with re-coding), a test for understanding logical-grammatical relations, recognizing time using a “blind” clock. Children in the main group made the following types of errors: topological (changes in the general scheme of the figure), metric (errors in estimating distances, angles and proportions), coordinate errors in the arrangement of an object (top-bottom and right-left). In Figure 4: 1 – recognition of time using a “blind” clock, (p <0.001); 2 – understanding of logical-grammatical constructions (p=0.5); 3 - copying a figure with 180º rotation; (p=0.265); 4 – copying a perspective drawing (house) (p=0.002).
The impairment of visual-spatial perception indicates weakness of the temporo-parietal-occipital regions of the brain, which may lead to difficulties in learning geometry and stereometry in children.
Figure 4: The studying result of visuospatial function
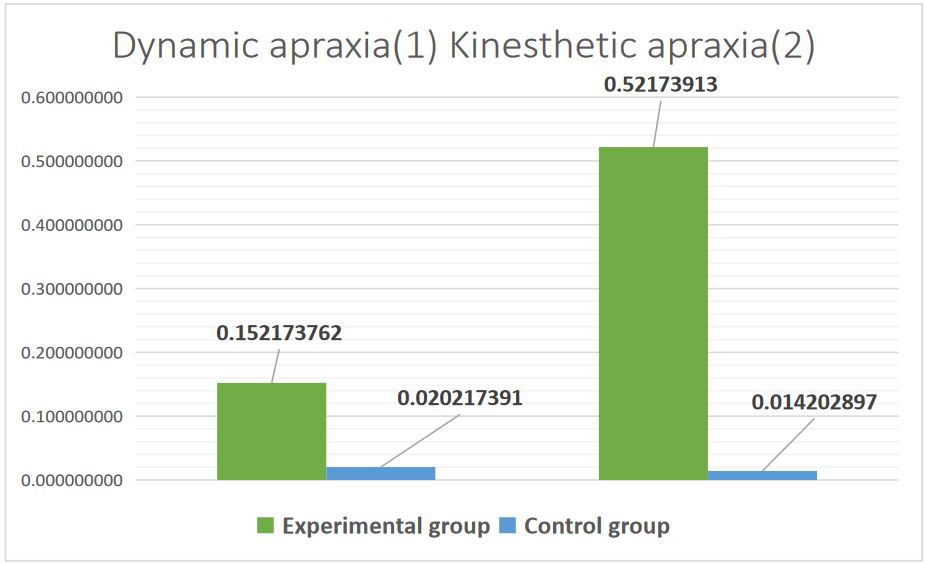
Study of motor functions (kinesthetic and dynamic praxis).
For the study of kinesthetic praxis, we used two-handed tests with visual control, and dynamic praxis, which was the “fist-edge-palm” technique. The analysis of the children's performance of these tests was carried out according to the following parameters: serial organization of movements, retention and assimilation of the motor program, the presence of perseverations and errors in the serial organization of movements. The severity of dynamic praxis disorders in children of the main group significantly exceeded that in the control group (p <0.001). In Figure 5: 1 - p=0.365; 2 - p=0.002.
The lesions were localized in convexital frontal parts of the brain under dynamic and regulatory apraxia. Kinesthetic apraxia results as a symptom of inferior parietal syndrome.
Figure 5: Study of motor functions
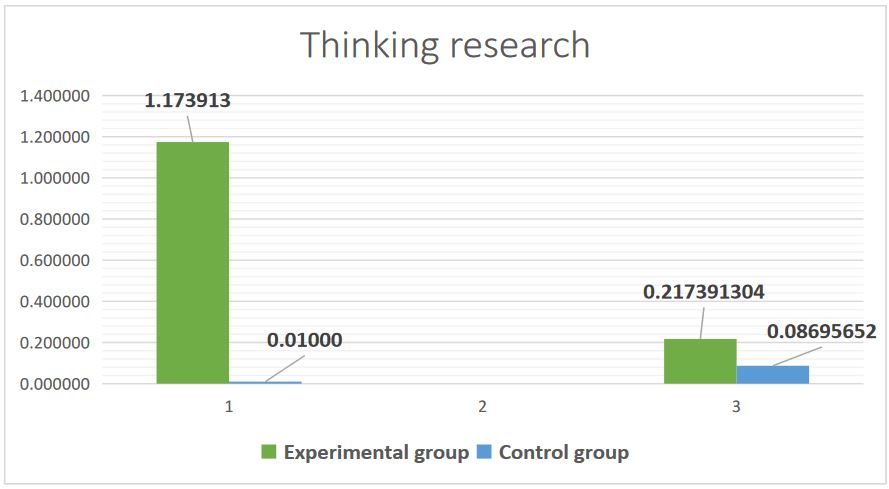
Study of thinking structure (verbal and non-verbal components).
When assessing verbal thinking, the following methods were used: composing a story based on story pictures (p <0.001), “Fourth extra” (p = 0.5). When assessing nonverbal thinking, tests for performing mathematical actions and operations; solving arithmetic problems (p=0.435) were used (Fig. 6).
The topical lesion in verbal thinking deficiency is prefrontal regions. For insufficiency of nonverbal thinking the damage location is in the temporo-parietal-occipital regions of the brain.
Figure 6: Study results of thinking
Study results of the emotional and personal sphere
Analysis of the study of the emotional and personal sphere in children with post-COVID syndrome using the Eysenck technique
Some children from the main group fall into the category with passive action, which correlates with a high level of neuroticism combined with introversion and deceit. Their lack of self-confidence can lead to withdrawal from communication, isolation, and complexes. Such children are afraid of making a mistake, to cause anger or displeasure of adults. Therefore, they may not answer the question even when they know the correct answer, and their deceit is associated with the desire to please the experimenter. In addition, these children may show aggressive behavior, which is a defense against their anxiety and self-doubt. In unfavorable circumstances, these children may develop depression and phobias, i.e. unmotivated fears (of darkness, heights, enclosed spaces, etc.).
Analysis of the study results of the emotional and personal sphere in children with post-COVID syndrome using the M. Lüscher color test
The core of M. Lüscher's concept comes from the assertion that all people (and more widely living organisms) live and act in approximately the same color environment. Therefore, a number of typical life situations occur when certain color tones dominate. For instance, we see the blue color of the sky in the vast majority of cases, being passive and inactive; red color (fire, blood, mature food, etc.), is generally combined with high activity of the subject, etc.
According to the principles of higher nervous activity, constant combination of certain colors with typical life situations leads to the association of color as an element of life situation, psychophysiological state, energy mobilization, and behavior stimulated by a given situation.
Figure 7: Basic colors of the Lüscher test.
The record of the subject's choices is made in conventional numbers: gray - 0, dark blue - 1, green - 2, orange-red - 3, yellow - 4, purple - 5, brown - 6, black - 7 (Fig. 7).
- If at least one of the primary colors is in the last three places of the color scheme, then it and the subsequent colors indicate a state of anxiety. The method of alarm compensation is determined by the characteristics of the color in the first position.
- If, in the presence of anxiety, one of the primary colors is in first place, then compensation is considered more successful than in the case of an additional one, which indicates the inadequacy and failure of compensatory behavior.
- The presence of gray, brown or black at the beginning of the color range indicates a negative view of life. If one of these colors stands on second or third place, it itself and all the colors to the left of it are considered as compensation.
Among children with post-COVID syndrome the two main colors stand in the last three places in 85% of cases. In 65% of cases, the presence of gray is at the beginning of the color scheme. Compensatory mechanisms are traced in 55% of cases.
Changes in the structure of the emotional sphere are a consequence of insufficiency of the limbic structures and the medio-basal frontal and temporal regions of the cerebral cortex. Lesions of medio-basal cortical sections are a part of the first (energetic) block. Damage to this cortical zone leads to the disruption of modally nonspecific factors, manifested in other disorders of mental functions.
Medio-basal sections of the temporal cortex are part of the limbic, which is characterized by very complex functions. These include regulation of the level of wakefulness, emotional states, memory processes, consciousness, etc. The lesion of temporal parts of the brain causes distinct emotional disorders, which are classified in the psychiatric literature as affective paroxysms (in the form of attacks of fear, sadness, horror), accompanied by violent autonomic reactions. These paroxysms usually precede (as an aura) general convulsive epileptic seizures. Long-term shifts in affective tone are also common. The nature of emotional disorders to a certain extent depends on the side of the lesion [23,26].
Complaints noted in children with post-COVID syndrome during classical neurological examination (taste and smell disorders were 32%; headaches - 12%; myalgia -8%; numbness or tremor of the hands - 8%; hand sweating -8%; dizziness or “darkening in the eyes” when tilting the head - 12%; weakness, fatigue, decreased tolerance to physical activity - 20%; memory impairment, decreased academic performance - 28%; mood swings, irritability - 8%, weather dependence - 8%, dyssomnias, weakness in legs, attention deficit, hyperkinesis - 4% each, persistent tremor of one hand in one case) also indicate the insufficiency of medio-basal parts, reticular formation, brain stem, basal ganglia, which provide energetic activation of brain activity and modally nonspecific brain functions.
Approaches to psychological correction of cognitive impairments in children with post-COVID syndrome
Neuropsychological rehabilitation is a complex medical-psychological-pedagogical impact on the defect, taking into account its mechanism, providing appeal to the patient’s personality, to the patient's small social groups (therapeutic group, family, work team), aimed at the restoration of higher mental functions as the main task, the solution of which allows to achieve the ultimate goal, the psychological rehabilitation of the patient, i.e. restoration of his personal and social status [29].
The main principles of correctional and developmental work are the following [30]:
- The principle of unity of diagnosis and correction
- The principle of normativity of development
- “Bottom-up” correction principle
- Principle of systematic development of mental activity
- Activity principle of correction
The development of rehabilitation programs for children with post-COVID syndrome, which is based on a comprehensive psychological assessment of the state of the cognitive and emotional spheres, taking into account the structural and functional features of the brain, requires multidisciplinary coverage and in-depth study of theoretical foundations and principles. We have outlined the main contours of this approach, which is the development of a correctional and developmental program. This program is aimed at activating the cognitive functions and emotional and personal relationships of children with post-COVID syndrome.
In developing effective treatment strategies for cognitive and emotional disorders as consequences of COVID-19 in children, we relied on both foreign scientific studies in recent years and Russian heritage. In the first case, we are talking about cognitive rehabilitation of children with an emphasis on cognitive remediation [31]. In the second case, we are talking about the Russian heritage – psychological and pedagogical [32, 33]. Thus, in the context of developing correctional-developmental programs that activate cognitive functions and correct emotional-personal relations of children with post-COVID syndrome, we rely on the theory of P.Ya. Galperin [33] about the “third type of learning”, about “cognitive motivation”, about the orientation basis of the child’s actions that determines learning. P.Y. Halperin's provisions are easily "read out" from the texts of authors who offer cognitive remediation programs for children before the "era" of COVID-19 and for children with post-COVID syndrome. It is about the principles of learning, about the so-called "strategic monitoring", directing the child's activity in the right direction, about reproducing the skill and transferring it into real, everyday life - in other spheres, and on other material [34, 35].
The correctional and developmental program, the contours of which we are developing, is basically developmental training that links together affective, cognitive and behavioral components, and includes various kinds of motivational reinforcements.
For example, speech function in ontogenesis is realized in three modalities: auditory-verbal, visual, and kinesthetic. Children with post-COVID syndrome were found to have impaired auditory-speech perception, which led to dysgraphia and dyslexia. To eliminate these defects, it is necessary to build a rehabilitation training program based on preserved functions through visual perception and kinesthetic praxis. In other words, to eliminate agrammatisms in writing, it is necessary to remove the use of dictations (auditory analyzer), and switch the training to visual perception (using tables and rewriting texts).
- Zhou J. Cognitive disorders associated with hospitalization of COVID-19: Results from an observational cohort study / J. Zhou, C. Liu, Y. Sun et al. // Brain Behav Immun. – 2021. – Vol. 91. – P. 383-392.
- Johns Hopkins Coronavirus Resource Center, COVID-19 Dashboard by the center of systems Science and Engineering (CSSE) at John Hopkins University (JHU), https://coronavirus.jhu.edu/map.html, September 20, 2020.
- Center of disease control and prevention, CDC COVID Data Tracker, https://covid.cdc.gov/covid-data-tracker/#demographics, Septermber 20, 2020.
- Coronavirus today [Electronic resource] // Coronavirus statistics. URL: https://koronavirus-today.ru (дата обращения: 28.11.2021.) Koronavirus-today//Statistics of koronavirus . URL: https://koronavirus-today.ru (In Russ)
- Woo M.S. Frequent neurocognitive deficits after recovery from mild COVID-19 / M.S. Woo, J. Malsy, J. Pöttgen et al. // Brain Commun. – 2020. – Vol. 2. – №2. – P. 1-9.
- Almeria M. Cognitive profile following COVID-19 infection: Clinical predictors leading to neuropsychological impairment / M. Almeria, J.C. Cejudo, J. Sotoca et al. // Brain Behav Immun Health. – 2020. – Vol. 9. – №16. – P. 1-5.
- C.C.-R. Team, Jorden M.A., Rudman S.L., Villarino E., Hoferka S., Patel M.T., Bemis K., Simmons C.R., Jespersen M., Iberg Johnson J., Mytty E., Arends K.D., Henderson J.J., Mathes R.W., Weng C.X., Duchin J., Lenahan J., Close N., Bedford T., Boeckh M., Chu H.Y., Englund J.A., Famulare M., Nickerson D.A., Rieder M.J., Shendure J., Starita L.M. Evidence for limited early spread of COVID-19 within the United States, January–February 2020. MMWR Morb. Mortal. Wkly. Rep. 2020; 69:680–684. [PMC free article] [PubMed] [Google Scholar]/
- Cheung E.W., Zachariah P., Gorelik M., Boneparth A., Kernie S.G., Orange J.S., Milner J.D. Multisystem inflammatory syndrome related to COVID-19 in previously healthy children and adolescents in New York City. JAMA. 2020; 324:294–296. [PMC free article] [PubMed] [Google Scholar]
- Dufort E.M., Koumans E.H., Chow E.J., Rosenthal E.M., Muse A., Rowlands J., Barranco M.A., Maxted A.M., Rosenberg E.S., Easton D., Udo T., Kumar J., Pulver W., Smith L., Hutton B., Blog D., Zucker H., New York S., C. Centers for Disease, T. Prevention Multisystem Inflammatory Syndrome in Children Investigation Multisystem inflammatory syndrome in children in New York State. N. Engl. J. Med. 2020; 383:347–358. [PMC free article] [PubMed] [Google Scholar].
- Feldstein L.R., Rose E.B., Horwitz S.M., Collins J.P., Newhams M.M., Son M.B.F., Newburger J.W., Kleinman L.C., Heidemann S.M., Martin A.A., Singh A.R., Li S., Tarquinio K.M., Jaggi P., Oster M.E., Zackai S.P., Gillen J., Ratner A.J., Walsh R.F., Fitzgerald J.C., Keenaghan M.A., Alharash H., Doymaz S., Clouser K.N., Giuliano J.S., Jr., Gupta A., Parker R.M., Maddux A.B., Havalad V., Ramsingh S., Bukulmez H., Bradford T.T., Smith L.S., Tenforde M.W., Carroll C.L., Riggs B.J., Gertz S.J., Daube A., Lansell A., Coronado Munoz A., Hobbs C.V., Marohn K.L., Halasa N.B., Patel M.M., Randolph A.G., C.-I. Overcoming, C.C.-R. Team Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 2020; 383:334–346. [PMC free article] [PubMed] [Google Scholar]
- Abdel-Mannan O., Eyre M., Lobel U., Bamford A., Eltze C., Hameed B., Hemingway C., Hacohen Y. Neurologic and radiographic findings associated with COVID-19 infection in children. JAMA Neurol. 2020 [PMC free article] [PubMed] [Google Scholar].
- Shweta Singh, Deblina Roy, Krittika Sinha, Sheeba Parveen, Ginni Sharma, and Gunjan Joshic Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020 Nov; 293: 113429. Published online 2020 Aug 24. doi: 10.1016/j.psychres.2020.113429 PMCID: PMC7444649 PMID: 32882598.
- Chen R., Wang K., Yu J., Howard D., French L., Chen Z., Wen C., Xu Z. The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in human and mouse brain. bioRxiv. 2020 2020.2004.2007.030650. [Google Scholar].
- Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Muller M.A., Drosten C., Pohlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020; 181:271–280. e278. [PMC free article] [PubMed] [Google Scholar].
- Sominsky L., De Luca S., Spencer S.J. Microglia: Key players in neurodevelopment and neuronal plasticity. Int. J. Biochem. Cell Biol. 2018; 94:56–60. [PubMed] [Google Scholar].
- Labo N., Ohnuki H., Tosato G. Vasculopathy and coagulopathy associated with SARS-CoV-2 infection. Cells. 2020;9 [PMC free article] [PubMed] [Google Scholar]/
- Teuwen L.A.,Geldhof V.,Pasut A.,Carneliet P COVID-19:the vascular unleashed. Nat.Rev. Immunol.2020;20:389-391/ [PubMed] [Google Scholar].
- Gulko E., Overby P., Ali S., Mehta H., Al-Mufti F., Gomes W. Vessel wall enhancement and focal cerebral arteriopathy in a pediatric patient with acute infarct and COVID-19 infection. AJNR Am. J. Neuroradiol. 2020 [PMC free article] [PubMed] [Google Scholar].
- Kaushik, Gupta S., Sood M., Sharma S., Verma S. A systematic review of multisystem inflammatory syndrome in children associated with SARS-CoV-2 infection. Pediatr. Infect. Dis. J. 2020 [PubMed] [Google Scholar].
- Hori H., Kim Y. Inflammation and post-traumatic stress disorder. Psychiatry Clin. Neurosci. 2019; 73:143–153. [PubMed] [Google Scholar].
- Abu-Rumeileh S., Abdelhak A., Foschi M., Tumani H., Otto M. Guillain-Barre syndrome spectrum associated with COVID-19: an up-to-date systematic review of 73 cases. J. Neurol. 2020 [PMC free article] [PubMed] [Google Scholar].
- Dalakas M.C. Guillain-Barre syndrome: the first documented COVID-19-triggered autoimmune neurologic disease: more to come with myositis in the offing. Neurol. Neuroimmunol. Neuroinflamm. 2020;7 [PMC free article] [PubMed] [Google Scholar].
- Luriya A. R. Higher cortical functions of a person and their disorders in local brain injury– StPb.: «Piter», 2008 (In Russ).
- Ahutina T.V. Polonskaya N.N., Yablokova L.V. Neuropsychological analysis of individual differences in children: evaluation parameters // Neuropsychology and psychophysiology of individual differences; under red. E.D. Homskoj, V.A. Moskvina. – Moskow-Orenburg, 2000. – p. 132-152. (In Russ)
- Balashova E.YU., Kovyazina, M.S. Neuropsychological diagnostics Classic stimuli materials. – 5-e izd.: Genezis. – M.- 2015.-70s (In Russ).
- Homskaya E.D. Neuropsychology 4-th. - StPb.: Piter, 2005. – 496 (In Russ).
- Lubov A. Troitskaya Neuropsychological evaluation of cognitive disorders in children after COVID-19/Lubov A. Troitskaya, Inga A. Plotnikova, Georgy G. Avakyan et al. // Eur J Transl Myol 32 (3): 10685, 2022 doi: 10.4081/ejtm.2022.10685
- Badalyan L.O. Children Neurology 2021.- 608p. ISBN 985-00030892-8 (In Russ].
- Cvetkova L.S. Neuropsychological rehabilitation of patients. Speech and intellectual activity. Study guide: MPSI, Modek, 2004.– 424s. (In Russ].
- - Troickaya L.A., Davidenko N.V. Practice for correction and development-training; theory and practice: Study methodic guide for students of high school; M, 2011.-104p. (In Russ].
- Hong H. T., Song S. I. Effectiveness of Computerized Cognitive Rehabilitation Therapy on Cognitive Function of Children with Disabilities: A Systematic Review //Journal of Mental Health Research in Intellectual Disabilities. – 2023. – p. 1-15. и др.
- Vygotskiĭ L.S. Ped M., Educational psychology. M.–Pedagogical. – 1991. (In Russ].
- Galperin P.YA. Methods for training and children intellectual growth and development. –M., MGU, 1985.
- Dickstein D. P. et al. Cognitive remediation: potential novel brain-based treatment for bipolar disorder in children and adolescents //CNS spectrums. – 2015. – Т. 20. – №. 4. – p. 382-390.
- Favre E. et al. Computer-based cognitive remediation program for the treatment of behavioral problems in children with intellectual disability: the «COGNITUS & MOI» study protocol for a randomized controlled trial //BMC psychiatry. – 2018. – Т. 18. – №. 1. – p. 1-7.