Liver neoplasms in pediatrics are rare but significant pathologies. Every year, about 175 thousand new cases of malignant neoplasms are diagnosed worldwide, of which liver tumors account for about 1.1%. Among them, hepatoblastoma, hepatocellular carcinoma and liver angiosarcoma are most often diagnosed [1]. One of the most aggressive and prognostically unfavorable malignant tumors of the liver is angiosarcoma, which accounts for less than 0.5% of all primary liver tumors in children [2]. Arising from the vascular endothelium, accompanied by early hematogenous and lymphogenous metastasis, the tumor has rapid invasiveness and high resistance to treatment. Liver angiosarcoma (LA) is most common in the adult population (60-70 years) and is associated with exposure to carcinogens (vinyl chloride, thorotrast, arsenic), while in pediatric practice it is even less common and has no established etiological factors [3]. According to the literature, LA can debut in infancy [4,5].
Diagnosis of LA in children is associated with significant difficulties due to the non-specificity of the clinical picture. As studies show, among the clinical manifestations of the disease, the most frequently recorded are abdominal pain, fever of unknown genesis and hepatomegaly, which in 70% of cases is initially interpreted as an infectious process or a benign neoplasm [4,6]. Cases in young children, including the neonatal period, where LA can imitate benign vascular malformations, present a particular diagnostic challenge [4]. The visual characteristics of LA have certain pathognomonic features. In computed tomography, the tumor appears as a heterogeneous formation with characteristic contrast and the presence of hemorrhagic cavities [7]. Magnetic resonance imaging demonstrates a hyperintense signal on T2-weighted images with areas of vascular voids, which reflects the angiogenic nature of the neoplasm [3]. However, these signs are not absolutely specific and require mandatory histological confirmation [5].
Histological diagnostics of LA is based on the identification of characteristic morphological signs: proliferation of atypical endothelial cells forming anastomosing vascular clefts and pronounced cellular atypia. Immunohistochemical examination plays a key role in differential diagnostics, demonstrating expression of vascular markers CD31, CD34 and ERG in 95-100% of cases. Determination of proliferative activity is of particular prognostic value: the Ki-67 index> 50% is associated with a particularly aggressive course of the disease and resistance to therapy. It is important to note that according to Fenn D. et al., 2024 [8], 30% of patients with LA develop consumptive hypothyroidism caused by tumor expression of type 3 deiodinase, which can serve as an additional diagnostic marker. Modern approaches to the treatment of LA in children are based on the principles of multimodal therapy, including surgery, chemotherapy and radiation therapy. The surgical component remains the cornerstone of therapy, with the radicality of resection (R0) being the most significant prognostic factor [9]. As studies demonstrate, organ-preserving resections using modern technologies, such as water-jet dissection (radiofrequency ablation and their combinations), allow achieving a 5-year survival rate of 65% of patients with localized forms [10]. However, it should be taken into account that 40-60% of patients already have distant metastases at the time of diagnosis, which requires a systemic approach to treatment [11].
Chemotherapeutic protocols for LA in children are mainly adapted from the regimens used for soft tissue sarcomas. The greatest efficiency is demonstrated by combinations based on anthracyclines and taxanes, in particular the CWS protocol, including vincristine, doxorubicin and cyclophosphamide in combination with paclitaxel [12]. According to the German CWS group, this approach allows achieving 5-year relapse-free survival in 64% of patients [11]. It is important to take into account that the use of paclitaxel in children is associated with a high risk of infusion reactions (up to 25% of cases), which requires careful monitoring and possible replacement with nab-paclitaxel [13]. A promising direction in the treatment of LA is targeted therapy, especially in the presence of specific molecular markers. As studies show, mutations in the PIK3CA genes, detected in 30% of patients, create the basis for the use of PI3K kinase inhibitors [14]. In addition, in some cases, antiangiogenic drugs (bevacizumab) and immune checkpoint inhibitors (pembrolizumab) demonstrate effectiveness, especially with PD-L1 expression [15].
However, the use of these methods requires further study in controlled clinical trials.
Aim: to demonstrate the capabilities of modern methods of oncosurgery in the treatment of metastatic angiosarcoma of the liver in children.
Clinical observation: A 6-year-old girl living in the Moscow region fell ill in December 2014, when she complained of abdominal pain not related to food intake, weakness, and temperature increases up to 39 ° C without any apparent reason. At the same time, the grandmother, while stroking the child's stomach, discovered a dense tumor in the abdominal cavity. This radial finding was the basis for the parents to consult a doctor. The girl was hospitalized in the gastroenterology department of the multidisciplinary city children's hospital. An ultrasound examination (US) revealed a tumor in the area of the right lobe of the liver. The child was transferred to the children's department of the Moscow Regional Oncology Dispensary for examination and treatment.
The child's condition upon admission was assessed as objectively severe in terms of the underlying disease. Abdominal palpation revealed a sharp increase in the liver, the dimensions of which were 16.0 x 8.54 x 16.75 cm. The lower edge of the right lobe of the liver was at the level of the crest of the wing of the right iliac bone. On contrast-enhanced computed tomograms, the liver structure is heterogeneous due to the presence of multiple volumetric multi-chamber formations with a cystic-solid structure, with a predominance of the cystic component, with dimensions from 2.67 x 4.5 to 5.11 x 9.14 cm. In S6 of the right lobe of the liver, there is a tumor node measuring 5.11 x 9.14 cm with a solid component, which most intensively accumulates contrast. The spleen has unclear internal contours, is enlarged to 9.49x3.96x3.43 cm, has a heterogeneous structure, with the presence of cystic-solid formations, ranging in size from 1.49 x 1.83 cm to 4.06 x 6.07 cm. In the projection of the left adrenal gland, a neoplasm is visualized, compressing the spleen and the upper pole of the left kidney, measuring 4.13x5.41 cm, identical in structure to neoplasms in the liver and spleen. Multiple para-aortic lymph nodes without clear contours are determined, merging into conglomerates, ranging in size from 1.04 x 1.49 to 1.81 x 2.32 cm.
At the end of December 2014, on 22.12.14, a fine-needle biopsy of the liver tumor was performed. Conclusion: cytogram of a non-epithelial malignant tumor of elongated spindle-shaped cells. The histological and immunohistochemical examination of the biopsy material allowed us to diagnose liver angiosarcoma (LA). Final clinical diagnosis: liver angiosarcoma, metastases in the spleen, para-aortic lymph nodes, stage IV. From December 26, 2014 to early June 2015, the child underwent 6 blocks of polychemotherapy according to the high-risk CWS protocol. The effect achieved was partial regression of the tumor and metastases. To perform the surgical stage of treatment, on July 6, 2015, the patient was transferred to the V.Y. Voyno-Yasenetsky Scientific and Practical Center of Specialized Medical Care for Children. The child's condition was objectively severe due to the underlying disease, but her health remained satisfactory: the girl was active, had no complaints, and her sleep and appetite were not disturbed.
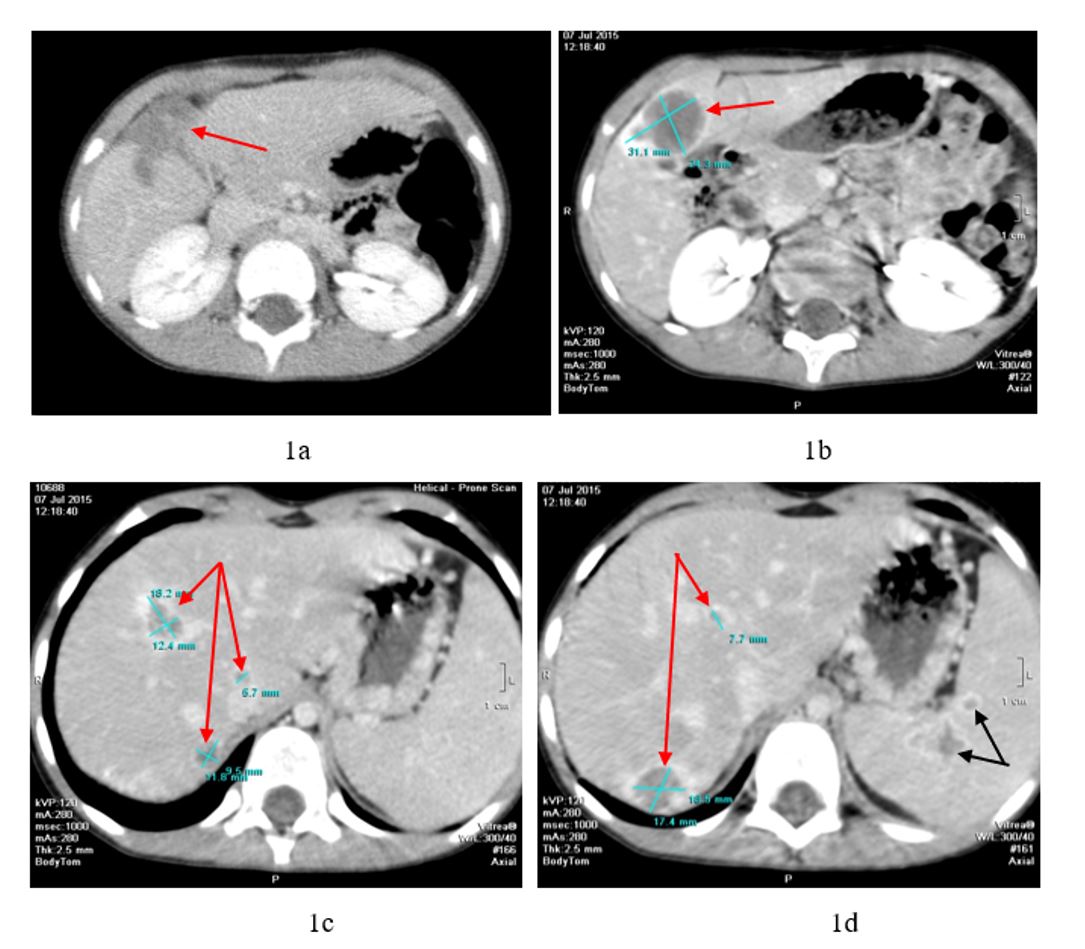
After discussing the child at an extended consultation of doctors, a decision was made to perform the 2nd stage of treatment - surgical in the amount of resection of all tumor foci in the liver, splenectomy, removal of metastatic lymph nodes. The CT data before the operation are presented in Figure 1. On contrast-enhanced computed tomograms, tumor nodes in the right lobe of the liver and the IV segment of the left lobe are clearly visible, intensively accumulating contrast (Figure 1 a, b, c, d). In addition, tumor nodes were detected in the area of the spleen parenchyma (Figure 1d).
07/14/15 surgery:
Stage 1: two-subcostal laparotomy, abdominal revision, bisegmentectomy (S5 and S6) of the liver, atypical resection of S4. Radiofrequency ablation (RFA) of all small-sized (no more than 2 cm) tumor foci in the liver with their subsequent removal (a total of 6 tumor nodes);
Stage 2: splenectomy with a part of the tail of the pancreas. Biopsy of lymph nodes suspicious for metastases.
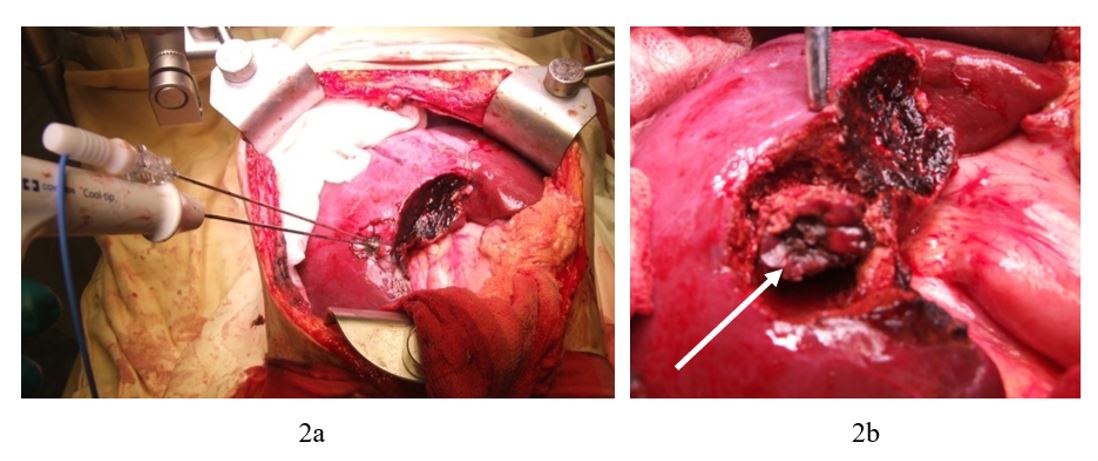
Stage 1 of the operation. The right lobe of the liver is mobilized after transecting the round and coronary ligaments. During revision, the tumor nodes are located in VI, VII, VIII and on the border of IV and V segments along the lower edge. A total of 6 tumor nodes were detected. The largest tumors - 3.5 cm in diameter, are located on the border of IV and V (along the lower edge), as well as in segment VII. The remaining four are in segments S6, on the border of S7 and S8 and segment S5. Atypical resection of the liver of segments S5, S6 and S7 was performed. The remaining 4 tumor nodes, up to 2 cm in size, were subjected to RFA, with their subsequent removal. Figure 2 shows the RFA stage of the tumor located in S7 of the liver. RFA and subsequent removal of the remaining three tumor nodes were performed in a similar manner.
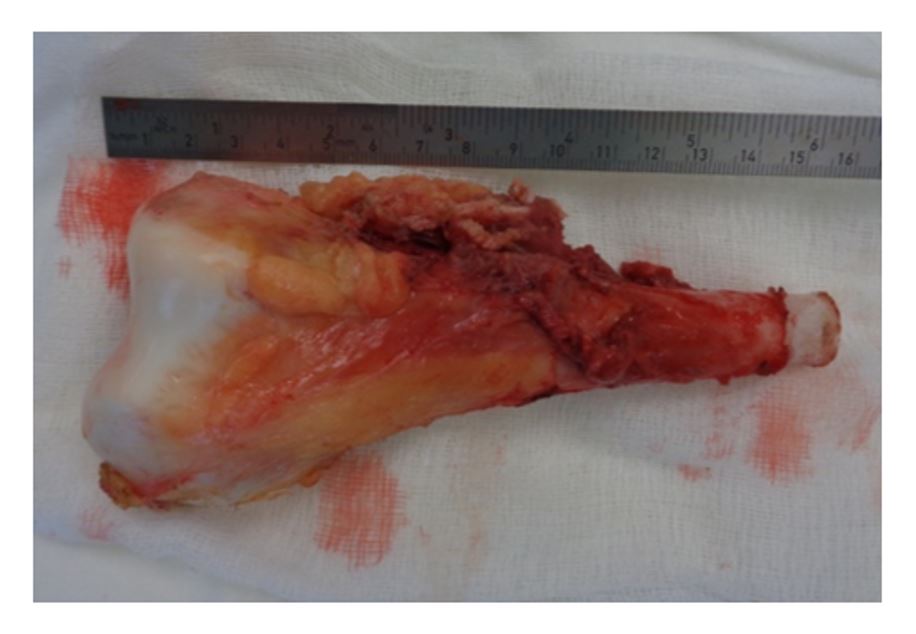
Stage 2 of the operation. When isolating the spleen from the surrounding tissues, it was found that the tail of the pancreas was fused to the spleen. In the middle section of the organ, two tumor nodes 1.0 and 1.5 cm in diameter were found. Resection of the tail of the pancreas was performed. The spleen was removed en bloc with a section of the tail of the pancreas. Retroperitoneal lymph nodes suspicious for metastatic lesions were taken for biopsy. There were no complications during the operation. The postoperative period was uneventful.
Histological conclusion: fragments of the liver, spleen, pancreas, lymph nodes and adipose tissue. All samples have necrotic fields surrounded by fibrous connective tissue with numerous histiocytes and hemosiderophages. There is no vital tumor tissue in the examined material. Histological picture of complete therapeutic pathomorphosis (IV degree). Thus, R0 resection is confirmed. Taking into account the results of histological and immunohistochemical analysis of the surgical material, a decision was made at a consultation of doctors to conduct adjuvant polychemotherapy according to the CWS protocol for the high-risk group.
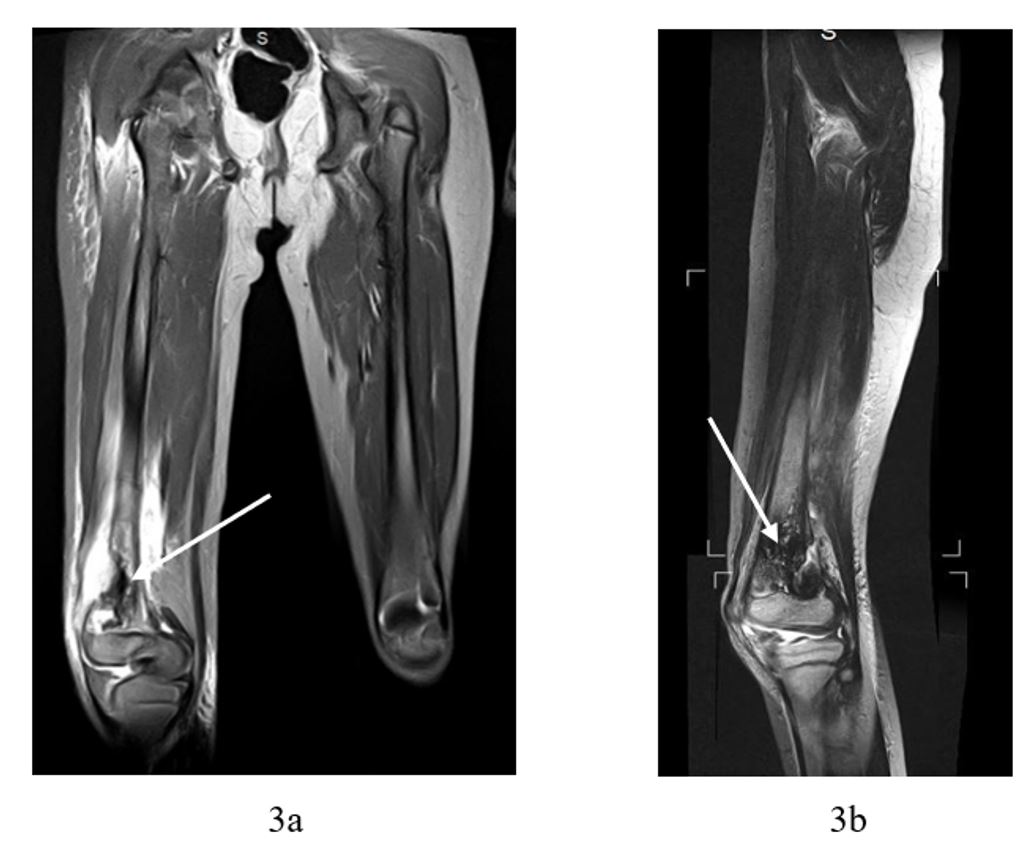
In October 2016, the girl began to complain of pain in the right hip. The patient underwent examination, including CT, magnetic resonance imaging (MRI) and biopsy of the lower third of the right femur (14.10.2016). Histological conclusion: elements of a malignant neoplasm with pronounced signs of low-grade atypia were detected. Morphological picture of angiosarcoma metastasis to bone. Since October 2016, a stage of anti-relapse chemotherapy has been performed. In response to the chemotherapy, a positive effect was registered in the form of a reduction in the size of the tumor of the right femur. MRI data before surgery are shown in Figure 3a, b.
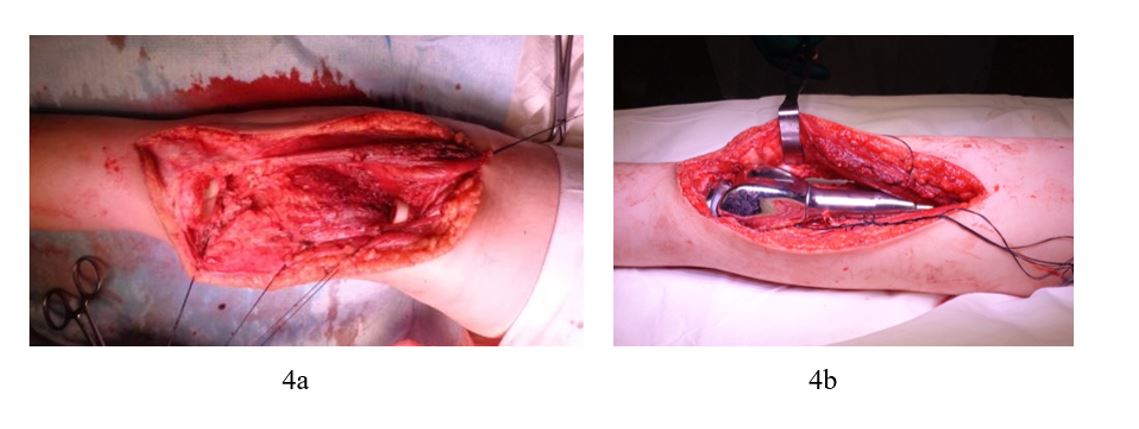
Considering the achieved effect of the chemotherapy on the right femur, the absence of recurrence of the liver tumor and other metastases, it was decided to perform an operation on the child in the amount of resection of the right femur with endoprosthetics of the knee joint. Based on the patient's age, it was decided to install a "growing" prosthesis (sliding) on the child.
22.12.2016 operation: distal resection of the right femur with knee joint endoprosthesis replacement with a "growing" endoprosthesis. The stages of the operation are shown in Figure 4 a, b.
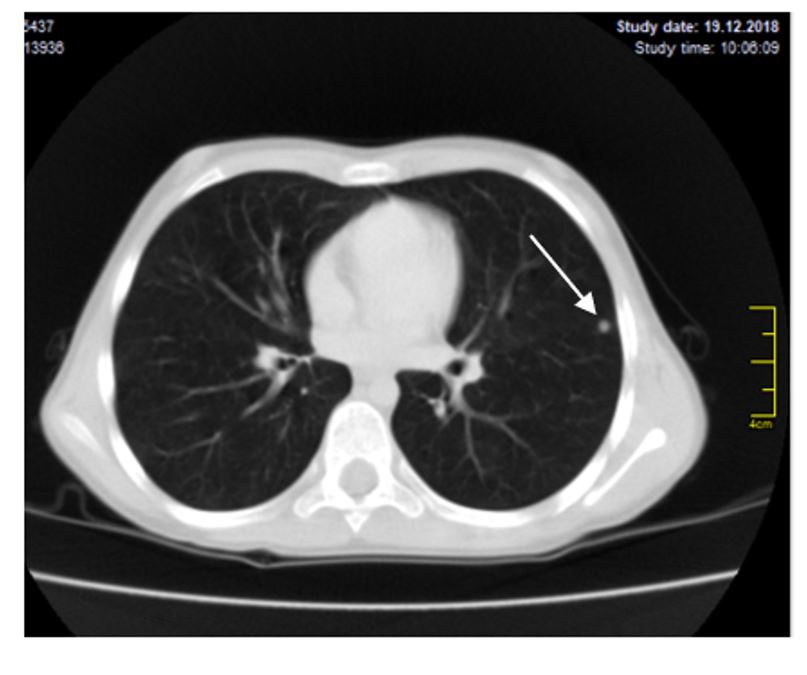
In the postoperative period, the girl received the necessary rehabilitation therapy, the result of which was the complete restoration of the function of the right leg: the patient walks independently, without support, there is no limp. From January to May 2017, the child underwent anti-relapse chemotherapy. The treatment was tolerated satisfactorily, without complications. In May 2017, antitumor treatment was stopped and the child was dynamically monitored. On December 19, 2018 (after 1.5 years), a control CT scan of the lungs revealed the presence of a focal neoplasm in S4 of the left lung, up to 3 mm in diameter (Figure 6).
During a comprehensive examination of the patient, no data were found for a local relapse of the disease in the liver, right femur, or the presence of metastases in organs and systems. At a consultation of pediatric oncologists and oncosurgeons, a decision was made to remove the metastasis from the left lung.
December 25, 2018 surgery: left thoracotomy, revision of the left lung, atypical resection of the upper lobe of the lung due to metastasis in S4. No other pathological changes were found in the lung. Histological and immunohistochemical examination of the removed area of the upper lobe of the left lung confirmed metastasis of angiosarcoma. From January 2019 to 09/24/19, the patient underwent anti-relapse cyclic program chemotherapy (6 blocks of chemotherapy).