Symptomatic Non-stenosed Carotid Artery causing progressive White Matter Disease Receiving Delayed Intervention
Roberta Potamianos1,2*, Michael Waters1,2 and Jim Jannes1,2
1The University of Adelaide
2Central Adelaide Local Health Network
*Corresponding author
*Roberta Potamianos, The University of Adelaide, Central Adelaide Local Health Network, 15 Stevenson Street, Nailsworth, 5058, SA
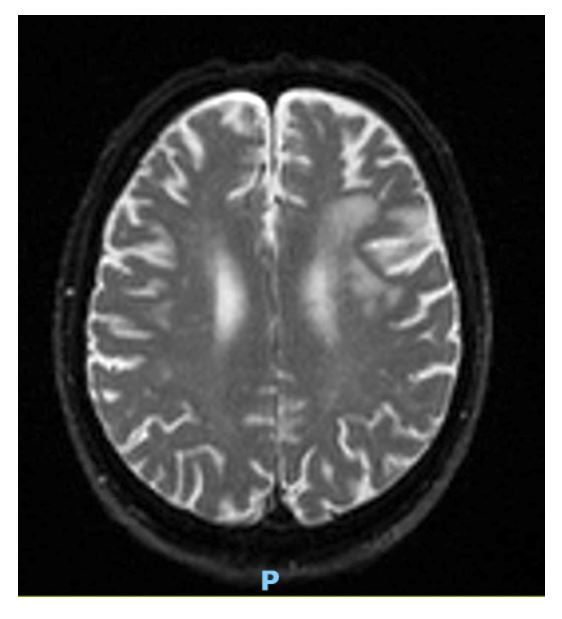
Figure 1: MRI Auto-Diff TRACEW revealing subacute white matter changes in L MCA territory from 4 years prior (2021 imaging).
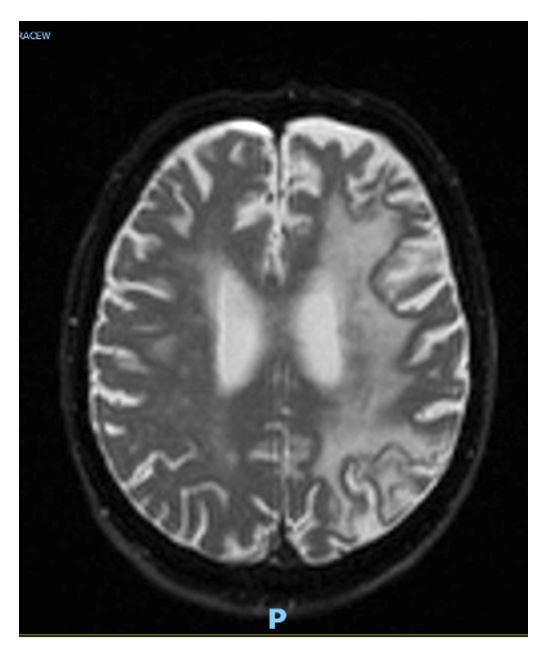
Figure 2: MRI – Auto-DIFF-TRACEW October 2024 at time of presentation demonstrating marked confluent L hemispheric white matter changes.
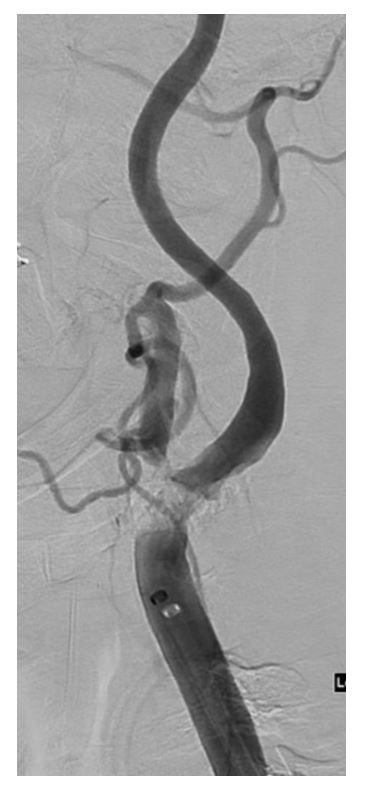
Figure 3: Digital Subtraction Angiography of Left ICA pre-stenting demonstrating heavily calcific, high grade stenosis.
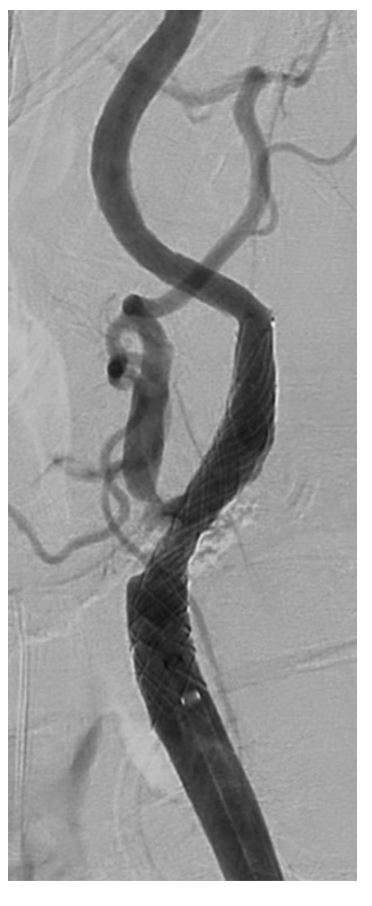
Figure 4: Digital Subtraction Angiography of Left ICA post-stenting.
- Lambert MP & Gernsheimer TB (2017) Clinical updates in adult immune thrombocytopenia. Blood. 129(21): 2829-2835.
- Cooper N, Ghanima W (2019) Immune Thrombocytopenia. N Engl J Med. 2019; 381(10): 945-955.
- Zhengrui X & Murakhovskaya (2023) Rituximab resistance in ITP and beyond. Immunol.
- Olson B et al. (2003) T-cell-mediated cytotoxicity toward platelets in chronic idiopathic thrombocytopenic purpura. Nature 9(9): 1123-1124.
- Qiu J et al. (2016) CD8+ T cells induce platelet clearance in the liver via platelet desialylation in immune thrombocytopenia. Rep p. 6.
- Al-Samkari H & Neufeld E (2023) Novel Therapeutics and Future Directions for Refractory Immune Thrombocytopenia. Br J Haematol 203(1): 65-78.
- Cooper N et al. (2022) Recent advances in understanding spleen tyrosine kinase (SYK) in human biology and disease, with a focus on fostamatinib. Platelets 34(1).
- Chen Y et al. (2024) A Novel Anti-CD38 Monoclonal Antibody for Treating Immune Thrmobocytopenia. N Engl J Med 390(23): 2178-2190.