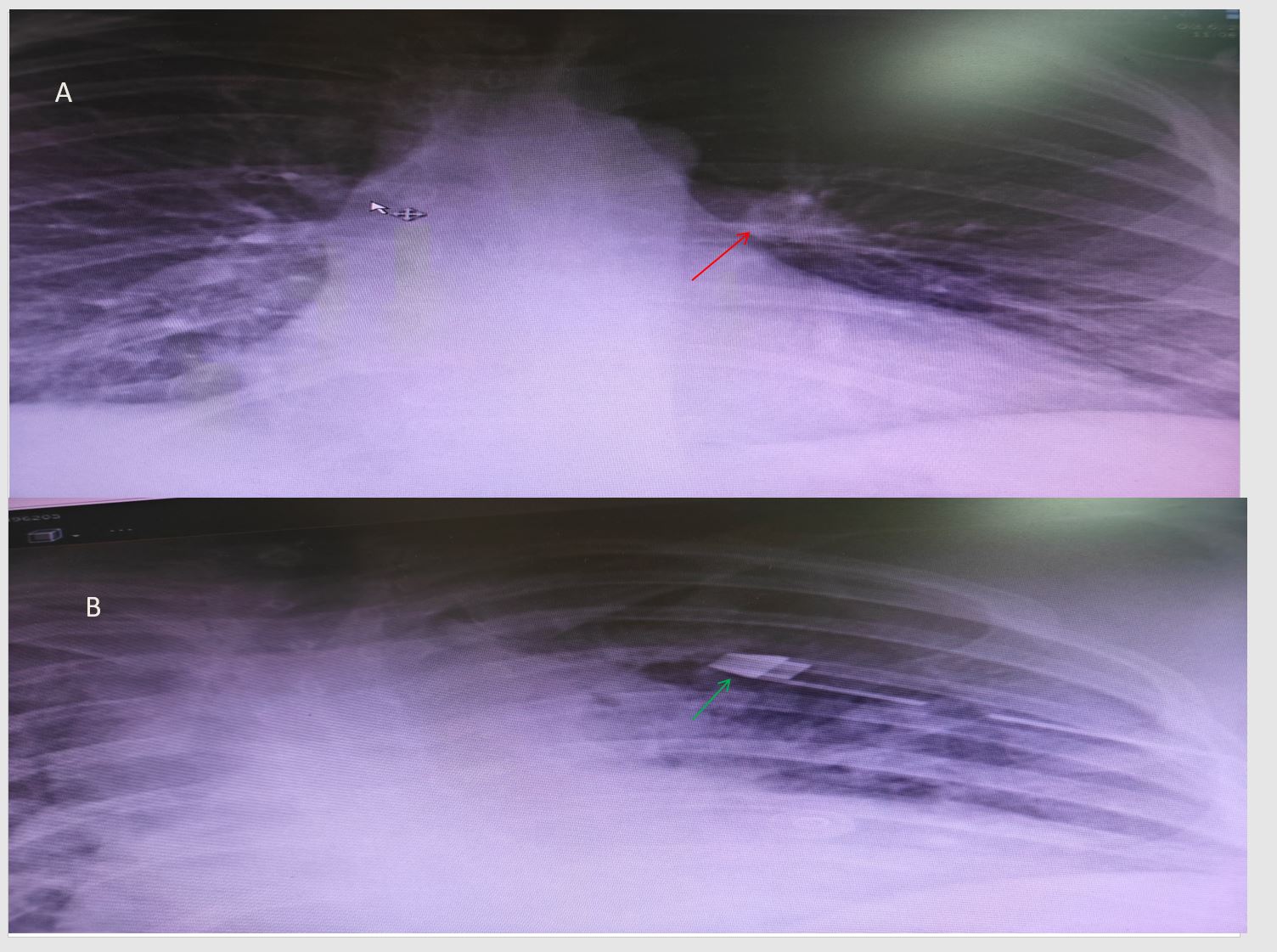
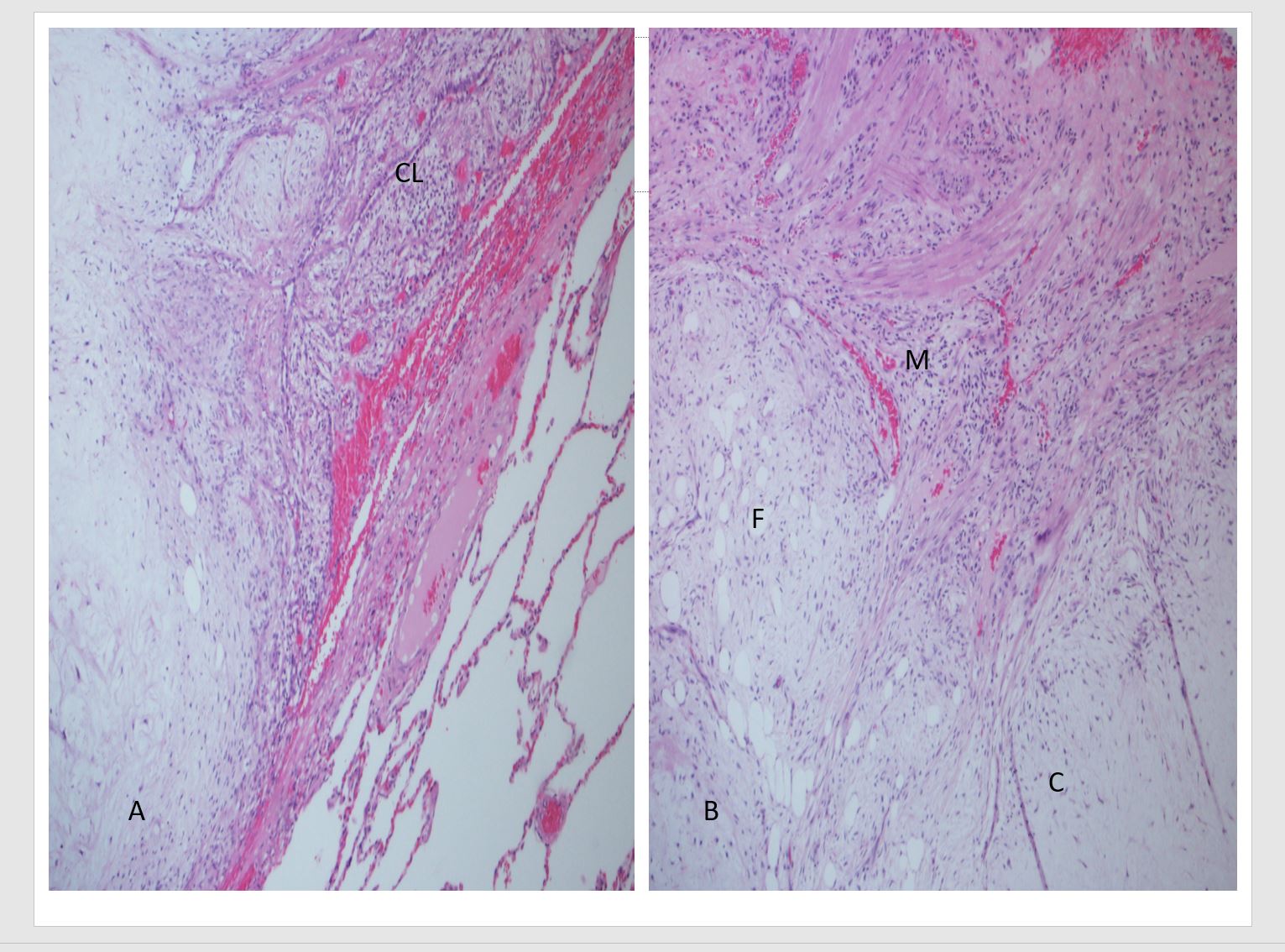
A lady aged 49 years had a referral appointment in the cardio-thoracic surgical unit at our hospital. Her reports disclosed that she was a treated case of right ovarian carcinoma 9 years ago, surgery followed by chemotherapy. No details were available regarding the type of cancer. Her regular follow-up CT (computed tomography) scan showed a lung nodule. With a high suspicion of the possibility of a metastatic tumour deposit in the lung, she was referred to our hospital for further management. Her only presenting complaint was shortness of breath on exercising. Other related respiratory symptoms like cough, hemoptysis, chest pain or paroxysmal nocturnal dyspnoea were all negative. Basic bloods and chest X-ray were done at our hospital. All blood tests including CBC (complete blood counts), LFT (liver function tests), RFT (renal function tests) and electrolytes were within the normal limits. Her PFT (pulmonary function test) spirometric values were within the acceptable normal range. Chest X-ray showed a lesion in the superior segment of the upper lobe of the lung measuring 1.2 cm (Figure 1). She agreed for the surgical excision of the lesion. Left VATS (video assisted thoracoscopic surgery) with bronchoscopy and left upper lobe superior segment resection were done. Frozen section was requested to look for grossly negative margins and not for tissue diagnosis on the fresh specimen. Fresh specimen received showed a nodule on slicing with adequate free margin. Lung tissue showed an irregular oval white glistening firm nodule measuring 1 cm across. Microscopic examination showed a lobulated mass of mixture of mature fat, smooth muscle and hyaline cartilage. Entrapped clefts lined by respiratory epithelium extending as slit-like spaces between the lobules were noted. No pleomorphism or necrosis or mitoses seen. Surrounding lung showed dilated alveoli and anthracotic pigment (Figure 2). It was a completely excised lesion with free margins. A diagnosis of pulmonary hamartoma {PH} was rendered.
No data is available regarding the tumor markers, and CT images were not uploaded into the patient’s file in our hospital.
Hamartoma definition by Albrecht – are tumor like malformations in which occurs only abnormal mixing of the normal components of the organ. The abnormalities may take the form of a change in quantity, arrangement or degree, or may comprise all three.[1]
Chondroid hamartoma, chondroid adenoma, mesenchymoma and pulmonary chondroma are the various terminologies for PH [1]. It is the commonest benign tumor of the lung with an incidence of 0.025 to 0.032% within the adult population [2]. Seen in 4th to 6th decade with greater prevalence in males with a ratio of 2-3:1 [3] Cases have been reported in younger age group and children as well.[4] Can be located anywhere in the lung but commonly close to the periphery beneath the pleura.[1] About 10% of them present endobronchially [2]. PHs are discovered incidentally on routine imaging and are asymptomatic except for endobronchial lesions. Chest X-ray and / or CT scans show coin shaped lesions with well-defined edges [2]. Popcorn or comma shaped calcification is pathognomonic for hamartomas [2]. Usually asymptomatic however, endobronchial lesions can present with cough, dyspnoea, pneumonia, hemoptysis or chest pain [3]. PH are slow growing and can be followed-up for any increase in the size of the lesion. Surgery is the treatment and curative indicated in fast growing, symptomatic and suspicious cases [4].
Grossly, they are lobulated, sharply delineated, glistening nodule of cartilage separated by ill-defined clefts.[1] Microscopy shows mixture of mature mesenchymal tissues in varying proportions. Tissues like fat, cartilage, bone, smooth muscle and fibromyxoid tissues are present. Cleft-like spaces are lined by respiratory epithelium. Malignant transformation is very rare.
Congenital aberrations with chromosome breakpoint at 6p21 in the high mobility group (HMG) gene is noted. PHs are a component of certain genetic syndromes like Carney’s triad and Cowden syndrome. Carney’s triad – PH + GIST (gastrointestinal stromal tumour) + functioning extradrenal paraganglioma.