Successful Surgical Repair of Pulmonary Artery Sling in a 10-Month-Old Infant: A Case Report
Oleksandr Romaniuk1,2, Dmytro Kryvolap1*,Illia Nechai1,Gorshkova1,Olena Dudko1and and Borys Todurov1,2
1Heart Institute of Ministry of Health of Ukraine, Kyiv, Ukraine
2Shupyk National Healthcare University of Ukraine, Kyiv, Ukraine
*Corresponding author
*Dmytro Kryvolap, Department of Pediatric Cardiac Surgery, Heart Institute of Ministry of Health of Ukraine, 5 A, Bratyslavska str, Kyiv 02166, Ukraine
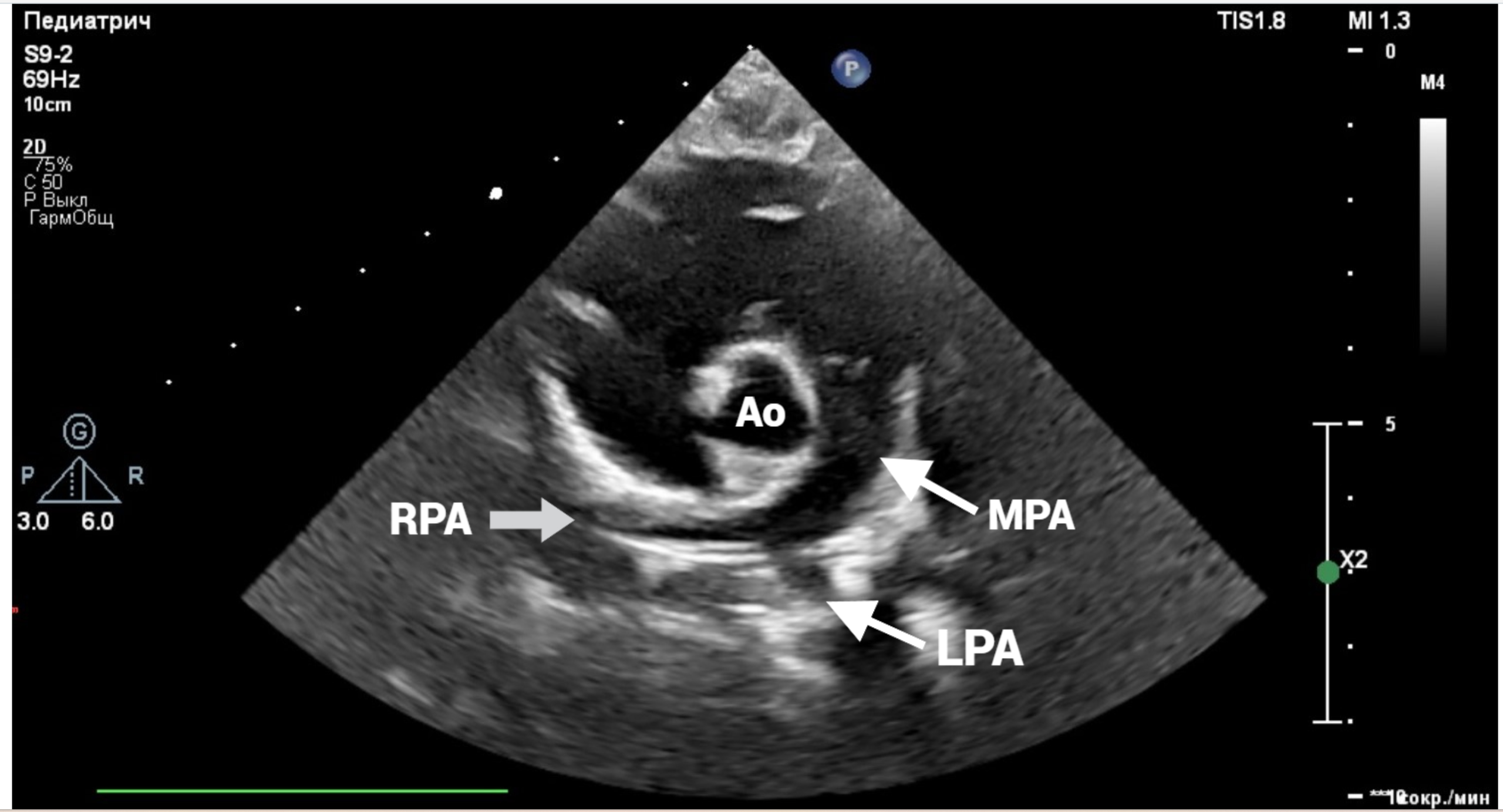
Figure 1: Echocardiography showing the abnormal origin of LPA from RPA. MPA, main pulmonary artery; LPA, left pulmonary artery; RPA, right pulmonary artery; AO, aorta.
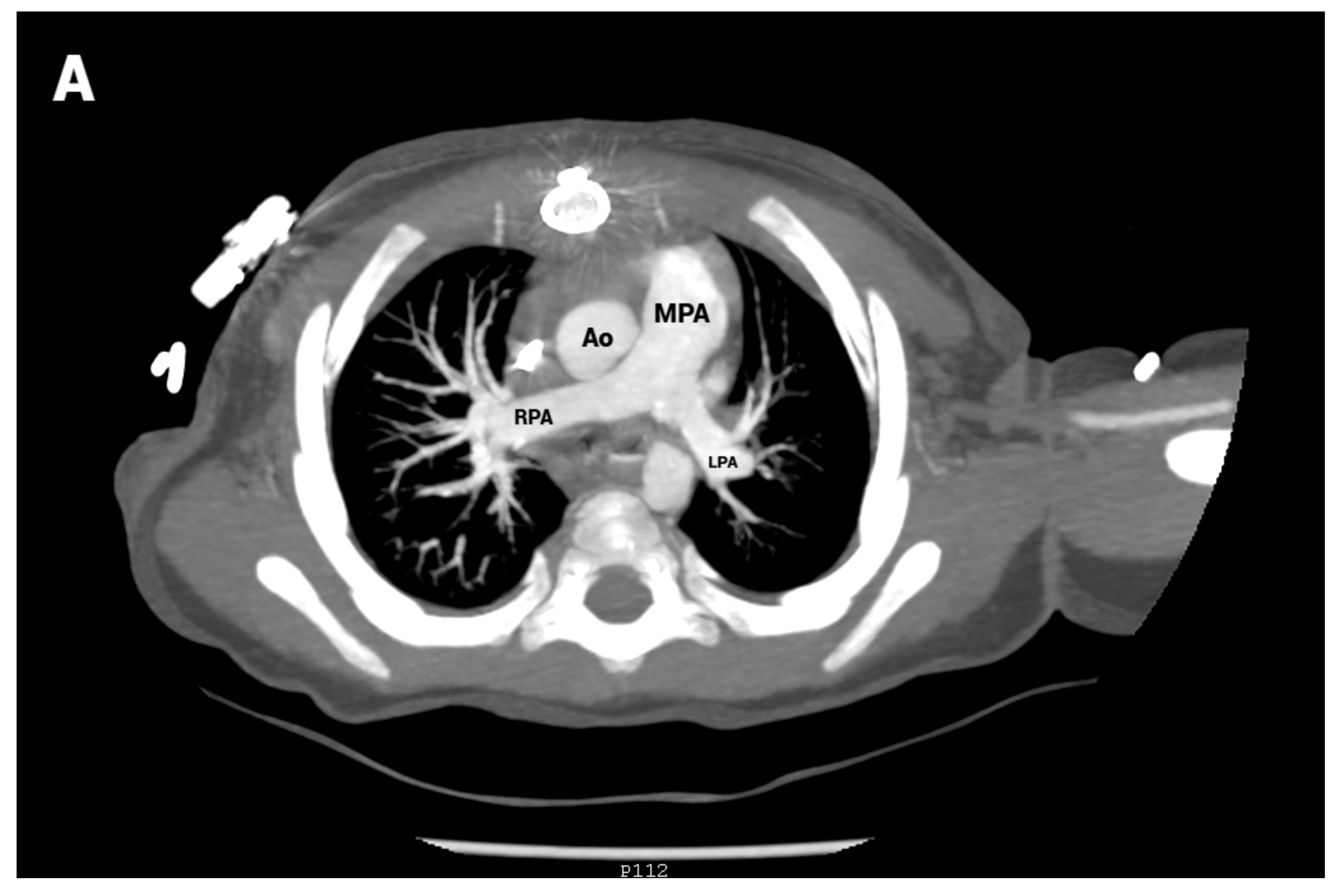
Figure 2: Pre-operative computed tomographic angiography (CTA) showing anomalous origin of the LPA from the posterior aspect of the RPA. The aberrant LPA runs behind the trachea as it courses to the left pulmonary hilum. MPA, main pulmonary artery; LPA, left pulmonary artery; RPA, right pulmonary artery; Ao, ascending aorta.
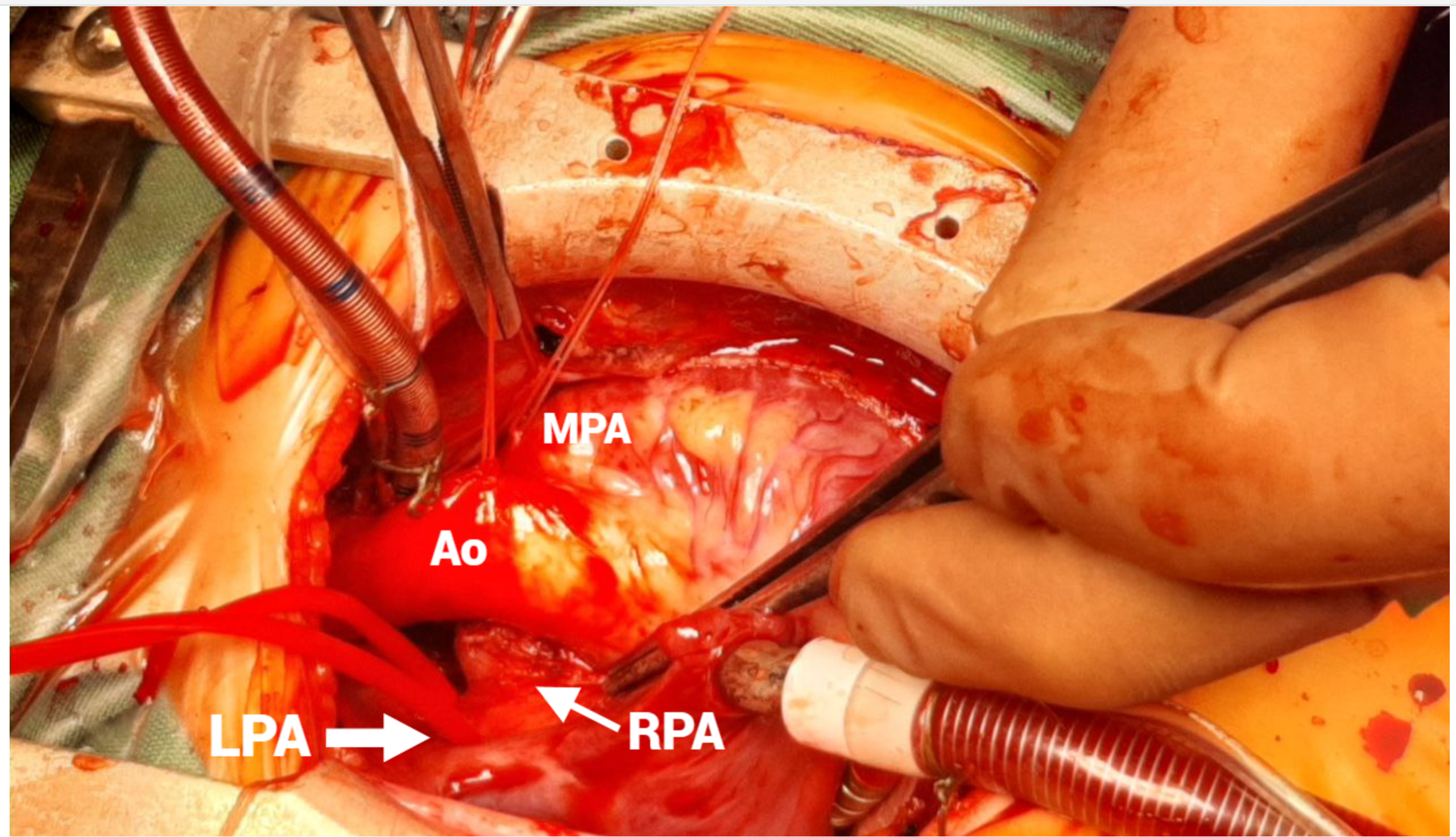
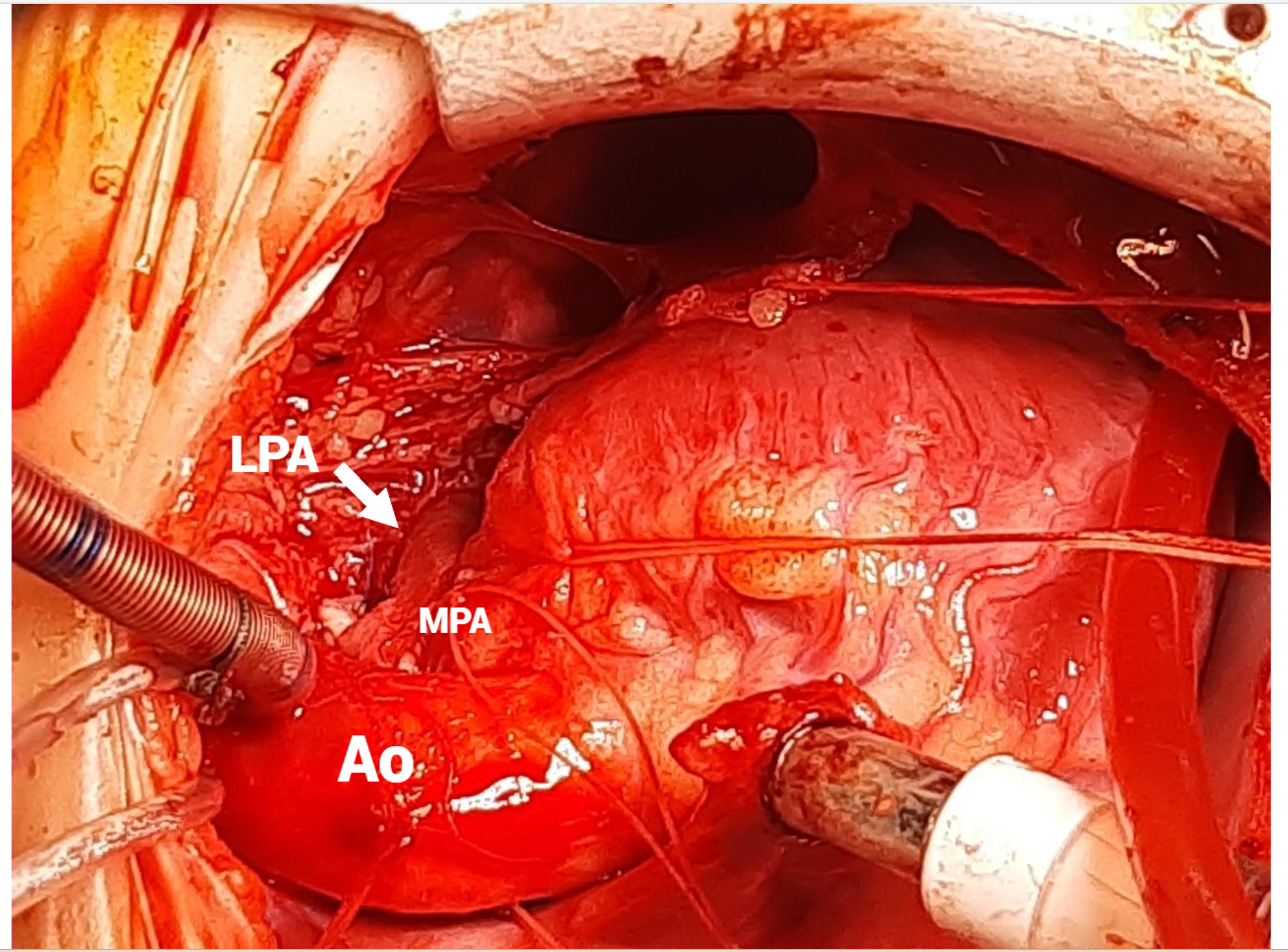
Figure 3:Intraoperative photo showing abnormal arising of the LPA from the RPA. MPA, main pulmonary artery; LPA, left pulmonary artery; RPA, right pulmonary artery; AO, aorta.
Figure 4:Intraoperative photo showing position LPA after reimplantation. MPA, main pulmonary artery; LPA, left pulmonary artery; AO, aorta.
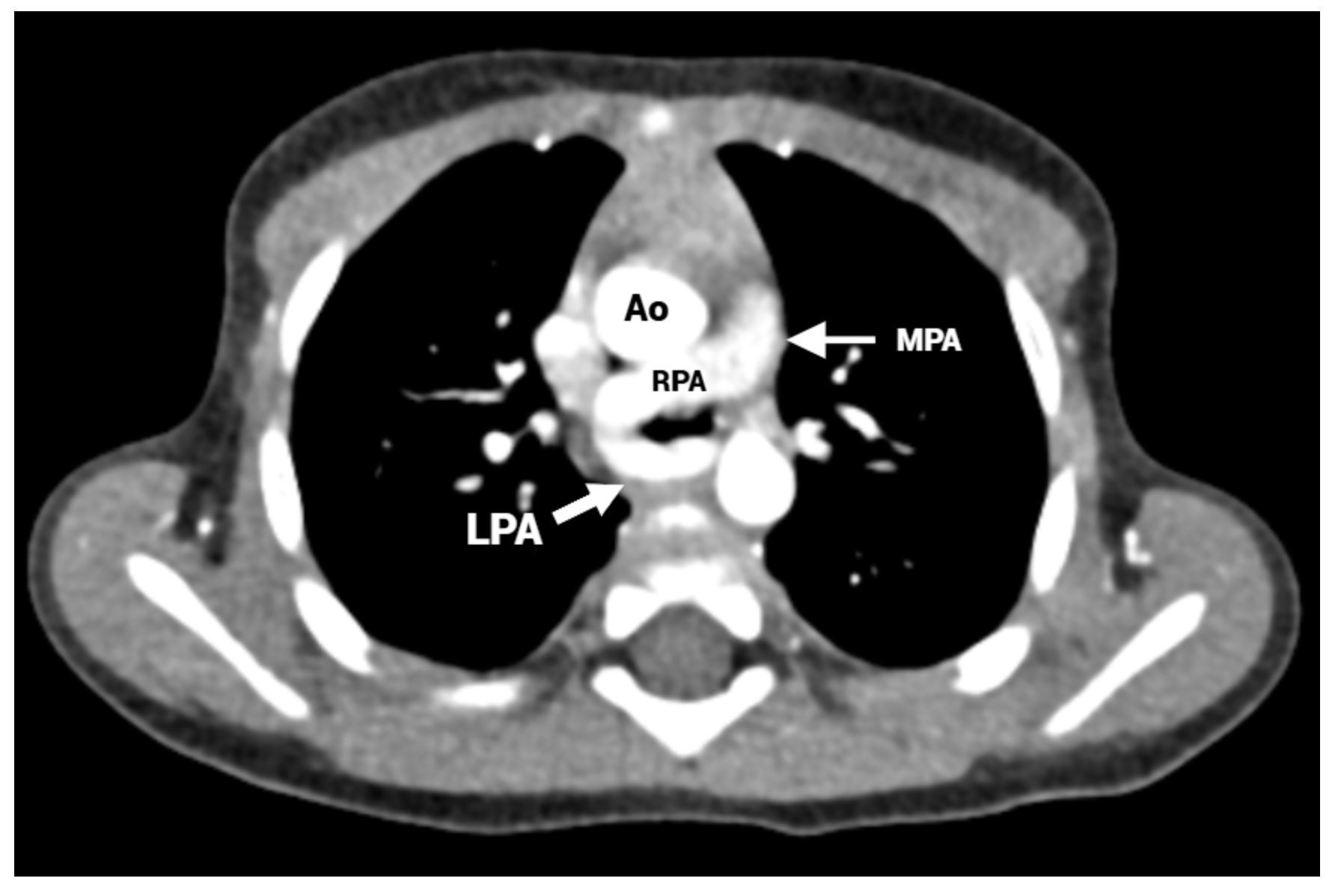
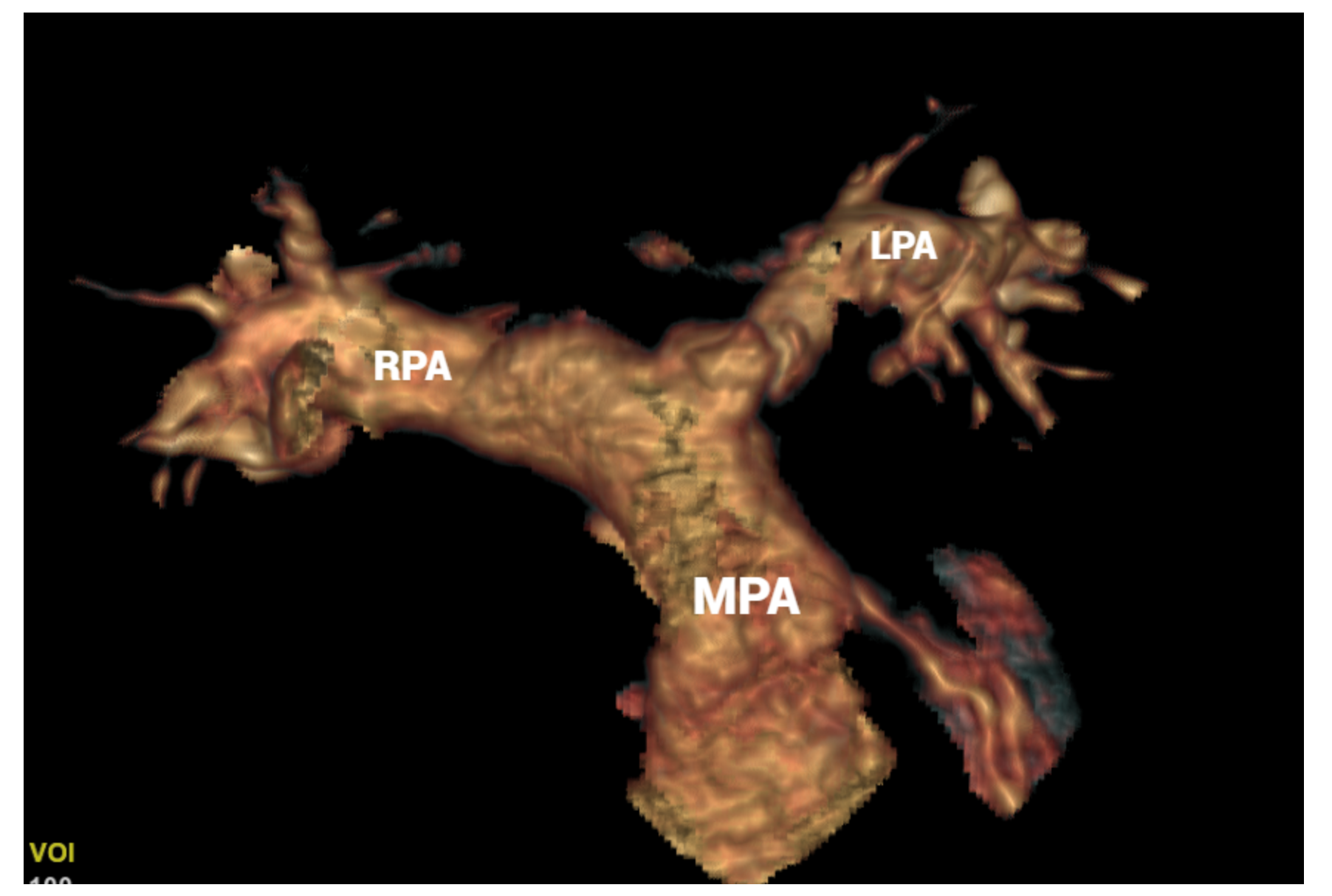
Figure 5: Post-operative CT angiography. (A) Axial image shows of the left pulmonary artery arising from the main pulmonary artery. (В) 3D image. MPA, main pulmonary artery; LPA, left pulmonary artery; AO, aorta.
- Wells TR, Gwinn JL, Landing BH, Stanley P (1988) Reconsideration of the anatomy of sling left pulmonary artery: the association of one form with bridging bronchus and imperforate anus. Anatomic and diagnostic aspects. J Pediatr Surg 23:892-898.
- Zhong YMM, Jaffe RB, Zhu M, Gao W, Sun AMM, Wang Q (2010) CT assessment of tracheobronchial anomaly in left pulmonary artery sling. Pediatr Radiol 40: 1755-1762.
- Lee KH, Yoon CS, Choe KO (2001) Use of imaging for assessing anatomical relationships of tracheobronchial anomalies associated with left pulmonary artery sling. Pediatr Radiol 31(4):269-278.
- Yu JM, Liao CP, Ge S (2008) The prevalence and clinical impact of pulmonary artery sling on school-aged children: a large-scale screening study. Pediatr Pulmonol 43: 656-661.
- Glaevecke H, Doehle H (1897) Über eine seltene angeborene Anomalie der Pulmonalarterie. Munch Med Wochenschr 44: 950-953.
- Potts WJ, Holinger PH, Rosenblum AH (1954) Anomalous left pulmonary artery causing obstruction to right main bronchus: report of a case. J Am Med Assoc 155(16): 1409-1411.
- Huang F, Lai QQ, Wu H, Ke XT (2021) A left pulmonary artery sling in an asymptomatic adult patient: a case report and review of literature. Heart Surg Forum 24: E278-E281.
- Yang CJ (2020) Bridging bronchus (pseudocarina) and left pulmonary artery sling: a case report and literature review. Int J Pediatr Otorhinolaryngol 136: 110158.
- Lee M (2023) A rare case of ring-sling complex in a symptomatic adult patient: a left pulmonary artery sling with complete tracheal rings. JRSM Open 14(11): 20542704231205388.
- Susanti DS (2024) Left pulmonary artery sling repair without cardiopulmonary bypass: a case report. Int J Surg Case Rep 118: 109692.